Enter Label: What if Bryan Johnson had Ovaries?
A convo about bio-hacking, fertility and the impact on longevity
Dear Companions,
If men had ovaries—or if Bryan Johnson did—we’d all be well aware of how improving fertility can increase longevity. The reproductive quest would be inextricably and publicly linked to the quest for a longer life. Yet, IVF and its health insights remain shrouded in mystery. We need a female Bryan Johnson to remedy that.
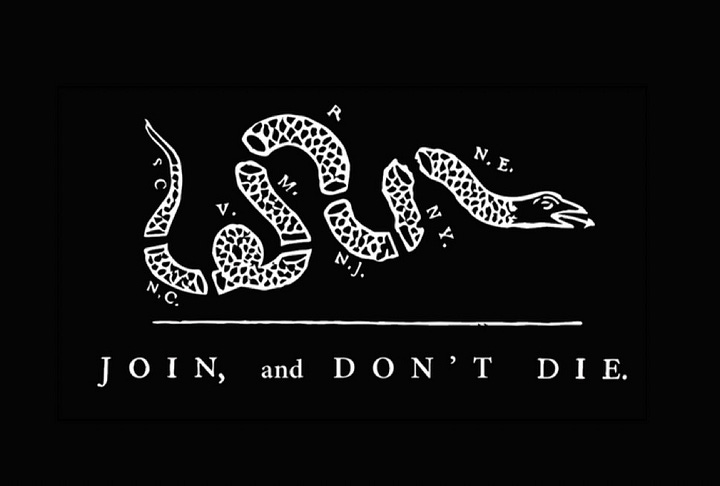
Johnson, a 47-year-old tech entrepreneur with 500,000 followers on X, is gaining attention for his "Project Blueprint," aimed at reversing his biological age through rigorous health regimens and experimental treatments. He is biohacking under the motto: Don't Die.
The challenge, scientifically, and philosophically, is that we can’t evaluate the success of Bryan Johnson’s longevity experiment until the end of his life—or lack thereof, I suppose. For discussions of infinity, David Deutsch is better at exploring this dilemma than I am.
But the female equivalent to Johnson demonstrates more immediate and measurable outcomes. An IVF woman knows within two cycles or three months of preparation due to the 90-day egg development. Results are observable through ultrasound follicle counts, hormone blood panels, and conception. In this world, 40–45-year-old women, far past the standard age for geriatric pregnancy, have children, which is at least just as impressive as Bryan Johnson’s sleep score.

In short, while admirable, Bryan Johnson’s markers are debatable, and getting hit by a bus might ruin his experiment. But follow a woman—Brianna Janson—trying to improve her fertility quickly, and you discover certainty in immortality magic today.
The ovary as a window into longevity
The ovary’s potential to illuminate aging mechanisms is supported by its status as the body’s fastest-aging organ. Ovarian aging involves a gradual decline in oocyte quantity and quality, leading to menopause. Studying this process provides real-time insights into broader mechanisms and how to reverse biological clocks.
"Menopause has long been viewed as an immutable inevitability. In fact, across the animal kingdom, menopause is the rare exception, occurring in humans and great apes and a few species of whales. Just as we are trying to extend the lifespan of other organs, like the heart and brain, we may be able to extend the lifespan of the ovary and thereby extend the widespread health benefits that the ovary provides.
-Dr. Zev Williams, chief of the division of reproductive endocrinology and infertility at Columbia University Fertility Center,
Although IVF has specialized hormonal protocols, many supplements used in fertility regimens overlap with Bryan Johnson’s Don’t Die protocol—dosages notwithstanding.
This overlap exists because fertility and longevity science are driven by similar principles. Enhanced mitochondrial health improves fertility and lifespan; better sleep supports both; and strong oxidative support preserves egg quality and counters aging.
"If we can extend the lifespan of the ovary, we may be able to extend the health benefits that the ovary provides, such a lowering the risk of heart disease and stroke, dementia, and osteoporosis."
What’s a biohacker?
A biohacker experiments with biology to enhance or modify the human body's functions. As you open the doors of possibility, you encounter different kinds:
Grinders: These biohackers focus on human augmentation by implanting devices under the skin or using technology to modify bodily functions.
Do-It-Yourself Biology (DIY Bio): This movement involves individuals and small organizations studying biology and life sciences using methods similar to traditional research institutions, often outside formal academic settings.
Nutrigenomics: Some biohackers explore how nutrition influences gene expression to optimize health through personalized dietary choices.
Quantified Self: This approach involves self-tracking biomarkers and behaviors to optimize health and performance.
But for all these categories, I have found what makes someone like Bryan Johnson hard-core is:
Extent and frequency of blood testing and measurement.
Range of supplements prescribed by a doctor or compounding pharmacy.
Time dedicated to the biohacking lifestyle.
Willingness to explore unconventional (n=1) approaches.
My journey
My biohacking journey is standard. As a young adult who didn’t want to rely on medicine, I dabbled in it. After Long Covid and total life dissolution, I went hardcore. I joined nearly 50 online groups for brain rewiring, blood testing, supplements, protocols, detoxes. I worked weekly with a functional doctor for 18 months. I found more experimental neurologists.
Many techniques I’ve written about—transcranial magnetic stimulation, functional neurology, supplements, hydration and pain reprocessing—come from that world. At nearly 41 years old, overwhelmed and doubtful now at the IVF clinic, I was curious about biohacking to augment results.
I plan to publish a 5-page biohacking protocol for Long Covid and general health.
What is a fertility biohacker?
Any woman undergoing IVF is a biohacker. She is modifying her natural abilities to conceive via assisted methods. She may have diminished ovarian reserve due to illness or age. She may be preserving options. Her partner may have poor sperm quality or be the same gender. She seeks to change this through intervention.
Her day-to-day resembles an intense Bryan Johnson acolyte. She undertakes 10+ blood draws in 30 days, uses tracking devices for ovulation and other markers, employs dietary restrictions to reduce inflammation, adopts better sleep management, and so on to enhance her fertility.
Baseline
The basic markers of any successful intervention determine the changes in follicle count and quality, providing indicators of treatment effectiveness.
Anti-Müllerian Hormone (AMH): Key hormone produced by ovarian follicles and an indicator of ovarian reserve, reflecting the remaining egg supply.
Follicle-Stimulating Hormone (FSH): This hormone regulates the menstrual cycle. Elevated FSH levels indicate diminished ovarian reserve.
Estrogen (Estradiol): This hormone is essential for developing and maintaining female reproductive tissues.
Antral Follicle Count (AFC): This is the number of small follicles in the ovaries via ultrasound. A higher AFC indicates better ovarian reserve and fertility potential.
These speak to egg quantity and likelihood of response to stimulation protocols. With respect to quality, the strongest measurable marker is retrieving the egg, pairing it with sperm, and sending it for Preimplantation Genetic Testing (PGT)—to screen embryos for genetic abnormalities before implantation.
Any measurable results will be found along these markers. For example, I saw two months of supplementing 5,000IU Vitamin D improved my AMH.
Additionally, there are peripheral results with overall health markers a biohacker might already be tracking. During stimulation, as my estrogen levels skyrocketed, my heart rate variability doubled, and my heart rate dropped to the 40s—a holy grail side effect for the sleep obsessed in Bryan’s world.
Like any medical field, conventional fertility spaces—especially larger IVF clinics—tend to be conservative. They provide limited and basic self-enhancement guidelines. After visiting three different clinics, I found all recommended the following basic adjuncts:
Prenatal Vitamins: A comprehensive prenatal vitamin containing essential nutrients such as folate, vitamin B12, vitamin B6, vitamin A, vitamin C, vitamin E, zinc, selenium, and iodine.
Coenzyme Q10 (CoQ10): 200 to 400 mg daily
Vitamin D3: 4,000 to 5,000 IU daily, especially if blood levels are below 40 ng/mL
Acupuncture: Regular sessions in the 3 months before IVF or conception attempts to improve blood flow to reproductive organs and reduce stress.
Surprisingly, they didn't discuss interventions like diet, except to suggest eating less processed foods. There wasn't much guidance on steps outside of stimulation protocols to induce the development of one more than one follicle for retrieval, which typically include:
Ovarian stimulation medications (gonadotropins: FSH, LH, or a combination)
GnRH antagonists or agonists (to prevent premature ovulation during stimulation)
Trigger injections (e.g., HCG or Lupron to mature and release eggs)
The second (and better) clinic I went to added in more medication: dexamethasone, a steroid, and Clomid, a medication that blocks estrogen receptors and tricks the body into thinking levels are lower during stimulation. Clomid is also used in weightlifting for men because it stimulates testosterone production by blocking estrogen receptors.
Moderate biohacking
A dedicated biohacker will explore beyond conventional advice, investigating interventions supported by emerging clinical evidence to enhance fertility. She will test more markers: fasting insulin, thyroid antibodies, and a wide range of immunological ones.
She will consult It Starts with the Egg by Rebecca Fett, a leading resource who recommends:
DHEA (Dehydroepiandrosterone): 25 mg three times daily (totaling 75 mg per day) or 25 mg per day.
Rationale: DHEA is a hormone precursor produced by the adrenal glands, used by the ovaries to synthesize estrogen and testosterone. Supplementation is recommended for women with diminished ovarian reserve. Higher doses (75 mg daily) enhance ovarian function, while a 25 mg daily dose mimics natural production levels.
N-Acetyl Cysteine (NAC): 600 mg daily.
Rationale: NAC is an amino acid derivative that supports antioxidant defenses and improves egg quality. It reduces oxidative damage and helps replenish glutathione, the body's primary antioxidant.
Alpha-Lipoic Acid (ALA): 400-600 mg daily (standard form; lower doses for R-lipoic acid).
Rationale: ALA enhances antioxidant protection by recycling CoQ10, vitamin C, and vitamin E into their active forms and increasing glutathione levels. Found in mitochondria, ALA assists with energy production and protects mitochondria from aging.
Melatonin: 3 mg nightly at bedtime.
Rationale: Melatonin supports egg quality, as higher levels are naturally present in ovarian follicular fluid. High doses can negatively affect ovulation; thus, a 3 mg dose is advised.
Myo-Inositol: 4 grams daily.
Rationale: Myo-inositol benefits women with polycystic ovary syndrome (PCOS) or insulin resistance, improving ovulatory function. It's a sugar molecule that plays a significant role in glucose transport into cells.
Vitamin E: 200 IU daily.
Rationale: Vitamin E supports antioxidant defenses. As a fat-soluble antioxidant in nuts, seeds, and oils, it is vital for the natural antioxidant defense system in the ovaries. Sufficient vitamin E in follicles is associated with higher egg quality.
Vitamin C: 500 to 1,000 mg daily.
Rationale: Vitamin C enhances antioxidant protection. Follicles accumulate significant vitamin C, supporting progesterone production and safeguarding the ovaries.
Diet Recommendations:
Approach: Adopt a Mediterranean diet rich in fish, nuts, oils, and legumes, with limited red meat.
Rationale: The Mediterranean diet improves fertility outcomes due to its anti-inflammatory properties and nutrient-rich composition.
Read the book for specific recommendations. Some supplements should stop during IVF. There’s a chapter on those to avoid (e.g., resveratrol, turmeric, maca, high dose L-arginine, royal jelly, pycnogenol).
More information is emerging about men optimizing fertility. Avoiding hot baths, following certain ejaculation schedules, and taking multivitamins, CoQ10, NAC, and Alpha Lipoic Acid can improve fertility and health. For more male supplements, check out here.
Hardcore mode
Hardcore biohackers will try options almost universally criticized by conventional clinics. They’ll do mold and heavy metal testing, among others. Supplementation includes:
LDN is a prescription medication that combats addiction in high doses, but in low doses is an immune modulator that prevents the immune system from overreacting to the gut microbiome. It is popular in the Long Covid biohacking community.
Serovital/Omnitrope is an amino acid-based supplement that claims anti-aging effects by increasing the production of growth hormone.
PQQ is an antioxidant that enhances the production of new mitochondria and their energy output.
Red Light Therapy involves a device emitting specific red or infrared wavelengths, suggested to enhance mitochondrial function, increase blood flow, and reduce inflammation. However, it’s unclear if the red light can penetrate sufficiently to improve ovarian function.
PRP (platelet rich plasma) is injected into the uterus or ovaries to restore health and functionality. To perform this treatment, patients’ blood is processed to remove red blood cells, leaving a concentrated solution of growth factors.
NAD (nicotinamide) plays a vital role in energy production, and declining NAD levels are linked to aging, sparking interest. However, nicotinamide may inhibit sirtuins—enzymes associated with longevity—so further research is needed.
Carnivore Diet: Some experts suggest this restrictive diet of only animal products to balance hormones, reduce inflammation, and enhance fertility.
Rapamycin could decrease ovarian aging by 20% and extend female fertility by five years while promoting longevity, according to early results. The Columbia University Fertility Center launched a double-blind study for women aged 35-45 with a once-weekly dose of 5mg Rapamycin.
Interestingly, Bryan Johnson discontinued a larger dose of Rapamycin in his regimen, concluding it was harmful for longevity. Perhaps fertility science will reveal the proper dosing.
Criticism & Reality
People pursuing intense biohacking options are often more desperate. In fertility, this means that conventional methods have failed, or are trying. They are vulnerable to predatory practices exploiting their desperation or misleading health headlines (see
).But the reality is that in any health field, some people can’t wait for the next big study. Their risk profile is exaggerated by the biological clock.
The good news about biohacking is that practices that promote optimal health benefit fertility outcomes. Regardless of fertility, the individual still gains better health.
Except for the PRP method, most are financially feasible, and more and more state and federal regulations are supporting reduced costs in IVF.
The Implications of Assisted Reproduction on Longevity
The relationship between fertility and longevity is complex. Some studies suggest a trade-off where increased fertility is associated with a shorter lifespan. Conversely, other research indicates women who have children later in life live longer. Whether prolonged fertility directly contributes to longer lifespan or indicates underlying longevity remains unclear. This relationship should inspire research and interest among those pursuing extended lifespans.
Then there are the societal implications. If women—and men—can extend their fertile years by 10 to 20 years, this would reshape longevity discussions. At the least, it reinforces the motivation to pursue longer, healthier lives. The desire to see one’s children grow can drive longevity goals.
Given the global children’s crisis, measures to extend fertility may be more critical than longevity interventions. If population levels decline sharply, the vast investments—billions or trillions factoring in broader healthcare—would merely extend enjoyment by a few decades rather than sustaining society. Neglecting fertility in longevity discussions represents a missed opportunity for both women and men in their quest for longevity and vitality.
A Call for Brianna Jansons
Just as we still lack a female Joe Rogan—a frustration I’ve articulated before in seeking Jody Wogan—the absence of a female Bryan Johnson leaves a noticeable gap. A Brianna Janson wouldn’t just mimic Don’t Die strategies for women, but develop, publicize, and bio-hack fertility. She would have a high-risk tolerance and be willing to try experiments and use social media to discuss the pros and cons.
Despite representing daily miracles, IVF remains secretive and overshadowed by testosterone-fueled biohacking spaces. Imagine how different conversations about longevity, fertility, and societal health would be if this quiet revolution became mainstream, informed by rigorous experimentation and open dialogue. It’s not just about extending individual lifespans; it’s about reshaping our collective future. Overlooking fertility in longevity conversations isn’t an oversight—it’s a missed opportunity to redefine how long and meaningfully we live.
Leave a comment today to share your experiences or learn about mine. Let’s compare biohacking notes.
With much love from the Healingvrse,
Rebecca




If men had ovaries we'd have a cure for morning sickness and a way to give birth painlessly by now!
Rebecca. Thanks for the info .have you ever heard of detoxing the body by slowly carefully (with the rt dentist) getting rid of.root.canals and any mercury or toxic.fillings?.
Tried Nattokinase,(it isnt a specific to fertility but rather to get rid of micro blood clots) or Ivermectin and Fenben for healing, inflammations, unknown parasites or fungus, detoxing and reviving the fertility in both men and woman? Red Raspberry. Or Homopathics. ? Caullophyllum?.